“Universal Healthcare: Balancing Rights, Laws, and Access for All.”
The Pros And Cons Of Universal Healthcare: A Balanced Perspective
Universal healthcare remains one of the most debated topics in modern policy discussions, with strong arguments on both sides. Advocates argue that healthcare is a fundamental right and that a universal system ensures equitable access to medical services for all citizens. Opponents, however, contend that such a system could lead to increased government control, higher taxes, and potential inefficiencies in service delivery. As governments around the world grapple with the complexities of healthcare reform, it is essential to examine both the advantages and disadvantages of universal healthcare to gain a balanced perspective on the issue.
One of the primary benefits of universal healthcare is that it guarantees medical access to all individuals, regardless of their financial status. In countries with such systems, citizens do not have to worry about being denied treatment due to an inability to pay. This approach reduces disparities in healthcare access and ensures that low-income individuals receive the same level of care as those with greater financial resources. Furthermore, universal healthcare can lead to improved public health outcomes by encouraging preventive care. When individuals have access to regular check-ups and early treatment, the overall burden of disease decreases, leading to a healthier population and reduced long-term healthcare costs.
In addition to promoting health equity, universal healthcare can also contribute to economic stability. In nations where healthcare is tied to employment, losing a job often means losing access to medical care. A universal system eliminates this concern, allowing individuals to seek medical attention without fear of financial ruin. Moreover, businesses benefit from such a system as they are relieved of the burden of providing private health insurance to employees, potentially leading to increased economic productivity and competitiveness.
Despite these advantages, critics argue that universal healthcare comes with significant drawbacks. One of the most frequently cited concerns is the potential for increased government spending and higher taxes. Funding a universal system requires substantial financial resources, which often necessitates higher taxation on individuals and businesses. Some argue that this could place an undue burden on taxpayers and lead to economic inefficiencies. Additionally, government-run healthcare systems may face challenges related to bureaucracy and inefficiency, potentially resulting in longer wait times for medical procedures and limited availability of specialized treatments.
Another concern is the potential impact on medical innovation. In countries with private healthcare systems, competition among providers often drives advancements in medical technology and treatment options. Critics worry that a government-controlled system could reduce incentives for innovation, as profit motives may be diminished. Furthermore, some argue that universal healthcare could lead to a decline in the quality of care, as healthcare providers may face increased patient loads and limited resources, potentially affecting the level of attention and treatment each patient receives.
While the debate over universal healthcare continues, it is clear that both sides present compelling arguments. The challenge for policymakers is to find a balance between ensuring access to healthcare for all citizens while maintaining efficiency, quality, and financial sustainability. As different countries experiment with various models of healthcare delivery, the ongoing discussion will shape the future of medical rights and access to care for generations to come.
Legal Rights And Healthcare: What The Law Says About Medical Access

Universal healthcare has long been a subject of debate, with legal frameworks playing a crucial role in determining access to medical services. The question of whether healthcare is a fundamental right or a privilege remains at the center of discussions, with laws varying significantly across different countries. In some nations, legal provisions guarantee healthcare as a right for all citizens, while in others, access depends on factors such as employment, income, or private insurance coverage. Understanding the legal foundations of medical access is essential in evaluating the broader implications of universal healthcare policies.
In many countries, constitutional provisions or statutory laws establish healthcare as a legal right. For example, nations with universal healthcare systems, such as Canada and the United Kingdom, have laws ensuring that all residents receive medical care regardless of their financial status. These legal frameworks are often supported by government-funded programs that allocate resources to healthcare services, ensuring that individuals do not face financial barriers when seeking medical treatment. In contrast, other countries, such as the United States, do not explicitly recognize healthcare as a universal right in their legal systems. Instead, access to medical services is largely determined by a combination of public and private insurance programs, with government assistance available primarily for specific groups, such as low-income individuals, the elderly, and veterans.
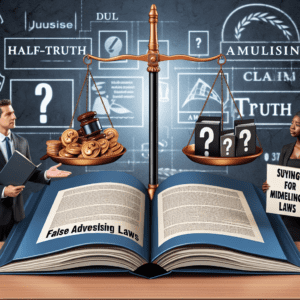
The legal debate over healthcare access often revolves around interpretations of constitutional rights and government responsibilities. Advocates for universal healthcare argue that access to medical services is a fundamental human right, essential for ensuring equality and social justice. They point to international agreements, such as the Universal Declaration of Human Rights and the International Covenant on Economic, Social, and Cultural Rights, which recognize healthcare as a basic human necessity. These legal instruments suggest that governments have an obligation to provide healthcare services to their populations, reinforcing the argument that medical access should not be contingent on financial means.
On the other hand, opponents of universal healthcare contend that mandating government-funded medical services may infringe upon individual freedoms and economic principles. They argue that a system based on personal responsibility and market-driven healthcare allows for greater efficiency, innovation, and choice. From a legal perspective, they emphasize that while certain rights, such as freedom of speech and due process, are explicitly protected in many constitutions, healthcare is not always included as a guaranteed right. Instead, they assert that governments should focus on creating policies that expand access without imposing universal mandates.
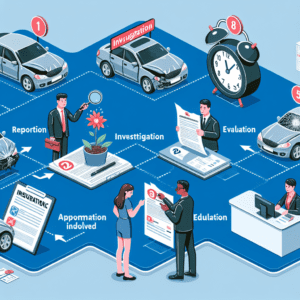
Legal challenges related to healthcare access often arise in the context of policy reforms and judicial decisions. In countries without universal healthcare, legal disputes frequently center on issues such as insurance coverage, medical costs, and government intervention in healthcare markets. Courts have played a significant role in shaping healthcare laws, determining the extent to which governments can regulate medical services and mandate coverage. For instance, in the United States, legal battles over the Affordable Care Act have highlighted the complexities of balancing individual rights with government responsibilities in healthcare policy.
Ultimately, the legal landscape surrounding medical access continues to evolve, influenced by political, economic, and social factors. As debates over universal healthcare persist, legal frameworks will remain a critical component in determining how societies address the fundamental question of whether healthcare should be a right or a privilege.
The Ethical And Economic Implications Of Universal Healthcare
Universal healthcare has long been a subject of intense debate, with discussions centering on both its ethical necessity and its economic feasibility. Proponents argue that access to healthcare is a fundamental human right, while opponents raise concerns about the financial burden such a system may impose on governments and taxpayers. As nations grapple with the complexities of healthcare reform, it is essential to examine both the ethical and economic implications of universal healthcare to understand its potential impact on society.
From an ethical standpoint, universal healthcare is often framed as a moral obligation. Advocates assert that healthcare should not be treated as a privilege reserved for those who can afford it but rather as a basic right that ensures the well-being of all individuals. The principle of justice supports this perspective, emphasizing that equitable access to medical services is necessary to prevent disparities in health outcomes. Without universal healthcare, lower-income individuals may struggle to afford essential treatments, leading to preventable suffering and even premature death. Furthermore, many ethical frameworks, including those based on human rights and social justice, argue that a society’s moral progress can be measured by how it cares for its most vulnerable members. By providing healthcare to all citizens, governments can fulfill their duty to protect public health and promote social equity.
However, the economic implications of universal healthcare present significant challenges. Critics argue that implementing such a system requires substantial government funding, which may lead to higher taxes or reallocation of resources from other public services. Additionally, concerns about efficiency and sustainability arise, as some fear that universal healthcare could lead to increased demand for medical services, longer wait times, and potential strain on healthcare providers. In countries with government-funded healthcare systems, such as Canada and the United Kingdom, reports of extended wait times for certain procedures have fueled skepticism about the effectiveness of universal coverage. Opponents also contend that government intervention in healthcare may reduce competition and innovation, potentially limiting advancements in medical technology and treatment options.
Despite these concerns, many studies suggest that universal healthcare can lead to long-term economic benefits. By ensuring that all individuals have access to preventive care, governments can reduce the overall cost of healthcare by minimizing the need for expensive emergency treatments and hospitalizations. When people receive timely medical attention, they are less likely to develop severe conditions that require costly interventions. Additionally, a healthier population contributes to a more productive workforce, which can enhance economic growth and stability. Countries with universal healthcare systems often experience lower healthcare expenditures per capita compared to nations with privatized systems, as administrative costs are reduced and pricing regulations prevent excessive medical charges.
Ultimately, the debate over universal healthcare requires a careful balance between ethical considerations and economic realities. While ensuring access to medical care aligns with principles of justice and human rights, policymakers must also address financial sustainability and system efficiency. As healthcare remains a critical issue worldwide, ongoing discussions and policy evaluations will be necessary to determine the most effective approach to providing equitable and affordable medical services for all.